Meniscal Surgery Linked to Higher Risk of Knee Arthritis and Cartilage Loss
Author: Radiological Society of North America (RSNA)
Published: 2014/12/04 - Updated: 2025/04/28
Publication Details: Peer-Reviewed, Findings
Category Topic: Surgery - Related Publications
Page Content: Synopsis - Introduction - Main - Insights, Updates
Synopsis: This research, presented at the annual meeting of the Radiological Society of North America, highlights that surgery to repair meniscal tears-a common orthopedic procedure-may significantly increase the risk of developing osteoarthritis and cartilage loss in the knee. The study analyzed data from the Osteoarthritis Initiative and found that 100% of knees that underwent meniscal surgery developed osteoarthritis within a year, compared to 59% of those with meniscal damage who did not have surgery. Furthermore, cartilage loss was observed in 80.8% of knees post-surgery, versus 39.5% in non-surgical cases.
These findings suggest that meniscal surgery, while often performed to alleviate pain and improve joint function, may actually accelerate joint degeneration, underscoring the importance of carefully evaluating surgical indications. Conservative management, including physical therapy and non-steroidal anti-inflammatory medications, is proposed as an alternative to surgery, especially for seniors and people with disabilities who are at higher risk for joint degeneration and may benefit from less invasive interventions - Disabled World (DW).
Introduction
A popular surgery to repair meniscal tears may increase the risk of osteoarthritis and cartilage loss in some patients, according to research presented today at the annual meeting of the Radiological Society of North America (RSNA).
The findings show that the decision for surgery requires careful consideration in order to avoid accelerated disease onset, researchers said.
Main Content
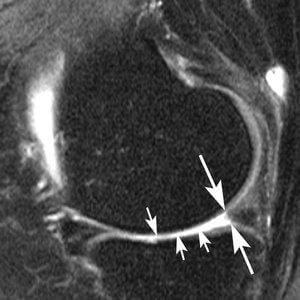
The new study focused on the meniscus, a wedge-shaped piece of cartilage in the knee that acts as a shock absorber between the femur, or thighbone, and tibia, or shinbone.
The two menisci in each knee also play an important role in joint stability.
Meniscal tears are among the most common knee injuries, and surgery is often performed to alleviate pain.

"Meniscal surgery is one of the most common orthopedic procedures performed to alleviate pain and improve joint function," said Frank W. Roemer, M.D., from Boston University School of Medicine in Boston and the University of Erlangen-Nuremberg in Erlangen, Germany. "However, increasing evidence is emerging that suggests meniscal surgery may be detrimental to the knee joint."
For the study, Dr. Roemer and colleagues examined data from the Osteoarthritis Initiative, a large, ongoing observational study of knee osteoarthritis incidence and progression.
Patients in the study were on average 60.2 years old and predominantly overweight, with a mean body mass index (BMI) of 28.3. Approximately two-thirds of the patients were women.
The researchers studied magnetic resonance imaging (MRI) exams of 355 knees that developed osteoarthritis during a five-year period, and a control group that was matched for age, gender, arthritic severity in both knees and BMI.
Of all knees, 31 underwent meniscal surgery during the year prior to the arthritis diagnosis, and 280 knees had signs of meniscal damage on MRI but did not have surgery.
Also part of the analysis were control cases with no meniscal damage.

The researchers assessed the risk of developing arthritis and cartilage loss during the following year for the different groups.
"We found that patients without knee osteoarthritis who underwent meniscal surgery had a highly increased risk for developing osteoarthritis and cartilage loss in the following year compared to those that did not have surgery, regardless of presence or absence of a meniscal tear in the year before," Dr. Roemer said.
All 31 of the knees that underwent meniscal surgery during the prior year developed osteoarthritis, compared with 165 (59 percent) of the knees with meniscal damage that didn't have surgery.
In addition, cartilage loss was much more common among knees that had undergone surgery. 80.8 percent of knees with surgery showed cartilage loss, compared with 39.5 percent of knees with meniscal damage and no surgery.
An alternative to surgery is conservative management. In conservative management, physical therapy is prescribed to help maintain and restore muscle strength and range of motion. Symptoms are commonly treated with ice and non-steroidal anti-inflammatory medications.
"The indications for meniscal surgery might need to be discussed more carefully in order to avoid accelerated knee joint degeneration," Dr. Roemer said.
Radiological Society of North America (RSNA)
RSNA is an association of more than 54,000 radiologists, radiation oncologists, medical physicists and related scientists, promoting excellence in patient care and health care delivery through education, research and techno-logic innovation.
Co-authors on the study are Ali Guermazi, M.D., Ph.D., C. Kent Kwoh, M.D., Michael Hannon, M.A., Jason Grago, M.A., and David J. Hunter, M.D., Ph.D.
Insights, Analysis, and Developments
Editorial Note: The implications of this research are particularly relevant as the population ages and the prevalence of knee injuries and osteoarthritis rises. For patients, especially older adults and those with disabilities, these findings support a more cautious approach to knee surgery, favoring conservative treatments when possible. Clinicians and patients alike should engage in shared decision-making, weighing the potential risks of accelerated arthritis against the expected benefits of surgery. As the evidence base grows, it becomes increasingly clear that not all knee injuries require surgical intervention, and a personalized, evidence-driven approach is critical to optimizing long-term joint health - Disabled World (DW).Attribution/Source(s): This peer reviewed publication was selected for publishing by the editors of Disabled World (DW) due to its relevance to the disability community. Originally authored by Radiological Society of North America (RSNA) and published on 2014/12/04, this content may have been edited for style, clarity, or brevity.